Squinting in children and teens can be more than a harmless habit—it often signals a vision problem that needs attention. For parents and caregivers, understanding the causes, solutions, and when to consult a doctor is vital for supporting healthy eye development. This article explores why kids squint, how to manage it, when to see a specialist, and whether glasses or surgery are the best options.
Squinting happens when kids narrow their eyes to improve focus, often due to blurry vision. This reflex reduces light and sharpens images temporarily. Here are the top reasons kids and teens squint:
- Refractive Errors:
- Nearsightedness (Myopia): Struggling to see distant objects, like a classroom whiteboard, is common in school-aged kids, leading to squinting.
- Farsightedness (Hyperopia): Difficulty focusing on close-up tasks, like reading, can cause squinting, especially during prolonged activities.
- Astigmatism: An irregularly shaped cornea or lens blurs vision at any distance, prompting squinting to clarify images.
- Strabismus (Misaligned Eyes):
- When eyes don’t align properly, kids may squint to correct double vision or focus with one eye. Strabismus can appear as one eye turning inward, outward, up, or down.
- Amblyopia (Lazy Eye):
- Weaker vision in one eye may lead to squinting as kids rely on the stronger eye to compensate.
- Eye Fatigue or Strain:
- Excessive screen time, dim lighting, or intense focus on close-up tasks can cause temporary squinting, especially in tech-heavy environments.
- Serious Eye Conditions:
- Rarely, squinting may indicate conditions like cataracts, glaucoma, or corneal issues, even in young people, requiring urgent evaluation.
- Environmental Triggers:
- Bright lights, glare, or uncorrected vision needs can prompt squinting as a reflex to improve clarity or comfort.

How to Manage Squinting at Home
Before assuming a serious issue, try these practical steps to address mild squinting:
- Optimize Lighting: Ensure proper lighting for reading or screen time. Reduce glare from windows or devices to ease eye strain.
- Follow the 20-20-20 Rule: Every 20 minutes, have your child look 20 feet away for 20 seconds to relax their eyes.
- Monitor Patterns: Note when squinting occurs (e.g., during homework, in bright light, or at school) to identify triggers.
- Encourage Open Dialogue: Ask your child about difficulty seeing, headaches, or eye discomfort, which often accompany squinting.
While these tips can help with minor issues, persistent squinting calls for professional care.
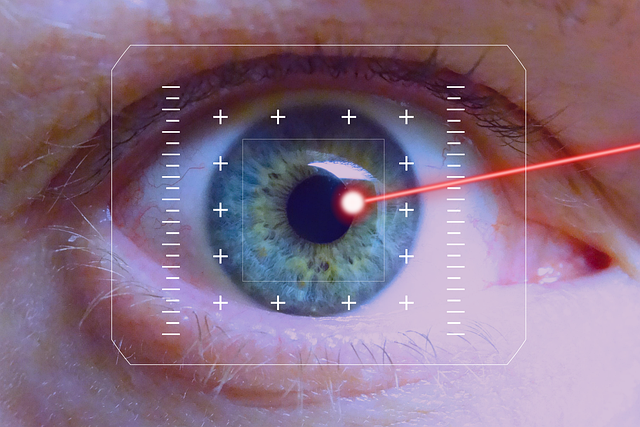
When to See a Doctor for Squinting
Early intervention is critical, especially in children, as their visual systems develop until around age 8–10. Book an appointment with a pediatric ophthalmologist or optometrist if you notice:
- Frequent squinting, especially during specific tasks like reading or watching TV.
- Misaligned eyes (strabismus) or one eye appearing weaker.
- Complaints of blurry vision, double vision, headaches, or eye pain.
- Squinting that persists beyond a few weeks or worsens over time.
- Family history of vision problems, as some conditions are hereditary.
A comprehensive eye exam can diagnose the root cause and guide treatment.
Treatment Options for Squunting in Kids
Treatment depends on the underlying cause of squinting. Here’s a look at common approaches:
- Glasses or Contact Lenses:
- For refractive errors like myopia, hyperopia, or astigmatism, prescription glasses or contacts often correct vision, eliminating the need to squint. Glasses are highly effective for most kids and teens, especially when diagnosed early.
- Specialized lenses, like bifocals or prisms, may be used for specific issues like strabismus.
- Vision Therapy:
- For conditions like amblyopia or mild strabismus, vision therapy involves exercises to strengthen eye muscles and improve coordination. This non-invasive approach can reduce squinting over time.
- Patching:
- In cases of amblyopia, patching the stronger eye encourages the weaker eye to develop, reducing squinting and improving vision.
- Surgery:
- Surgery is typically reserved for severe strabismus that doesn’t respond to glasses or therapy. It involves adjusting eye muscles to align the eyes properly. While effective, it’s not always the first choice and requires careful evaluation by a specialist.
- For rare conditions like cataracts, surgery may be needed to restore clear vision.
- Lifestyle Adjustments:
- Reducing screen time, improving lighting, and taking regular breaks can help with squinting caused by eye strain.
Can Glasses Correct Squinting, or Is Surgery Necessary?
In most cases, glasses effectively correct squinting caused by refractive errors, making them the go-to solution for myopia, hyperopia, and astigmatism. For amblyopia or mild strabismus, glasses combined with vision therapy or patching often work well. Surgery is typically a last resort for severe strabismus or other structural issues that glasses or therapy can’t address. An eye care specialist will determine the best approach based on the child’s condition and severity.
Final Thoughts: Act Early for Healthy Vision
Squinting in kids and teens is often a red flag for vision problems that, if caught early, can be effectively managed. Whether it’s a simpleც
System: simple pair of glasses or a more complex issue requiring surgery, addressing squinting promptly ensures better outcomes. Regular eye check-ups, especially for school-aged children, can catch issues before they worsen.
For personalized advice, consult a pediatric ophthalmologist or optometrist. Don’t wait—clear vision is key to your child’s learning, confidence, and quality of life.